The aftermath of acne often lingers long after the inflammation has subsided. For many, the visible reminders—scars, discoloration, and uneven texture—can weigh just as heavily on mental well-being as the initial breakouts. While countless treatments promise rejuvenation, one ingredient has consistently drawn the attention of dermatologists and skin care professionals alike: retinol. A derivative of vitamin A, retinol has become a cornerstone in dermatological regimens not only for aging but also for post-acne skin recovery. Understanding how retinol helps with acne scars involves exploring its biological mechanisms, therapeutic applications, and the evidence that supports its place in both over-the-counter and prescription treatments. The growing body of research and clinical experience continues to affirm retinol’s value in skin repair, placing it among the most trusted ingredients in dermatology today.
This article delves into the science, strategy, and practical advice behind using retinol for acne scars. It includes dermatologist-backed insights, current evidence, and expert perspectives to help readers better understand why retinol remains a go-to treatment for scar reduction, what makes the best retinol for acne scars effective, and how to integrate it safely into a long-term skincare plan.
You may also like: How to Choose Skin Care for Fine Lines: Evidence-Based Tips for Healthier, Younger-Looking Skin
Understanding Acne Scars: Why the Skin Struggles to Bounce Back
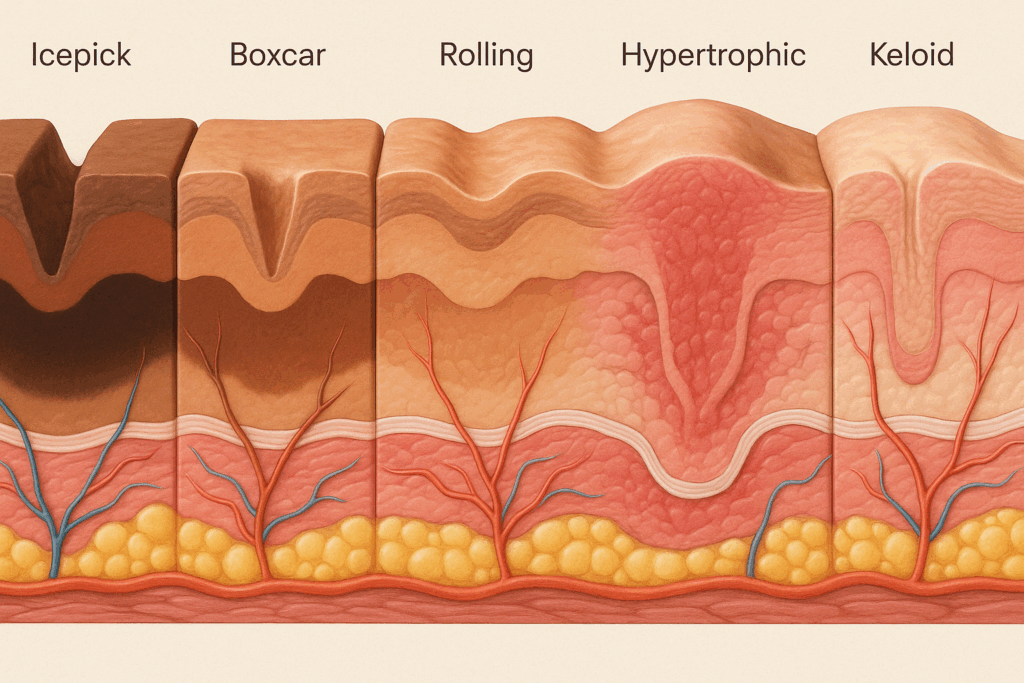
Before diving into treatment options, it’s important to understand what makes acne scars so persistent. Scarring occurs when inflammatory acne lesions—particularly cysts or nodules—penetrate deep into the skin, damaging tissue beyond the superficial epidermis. In response, the body tries to heal itself by producing collagen. However, this repair process is often imprecise. Too much collagen can result in raised scars (hypertrophic or keloid), while too little can cause depressed scars (atrophic scars, including icepick, boxcar, and rolling scars).
What complicates matters further is the role of melanin. Post-inflammatory hyperpigmentation (PIH), though not technically a scar, often accompanies acne, especially in individuals with medium to dark skin tones. The discoloration can persist for months or even years, creating additional emotional and cosmetic burdens. It’s within this complicated landscape of structural damage and pigmentation irregularities that retinol for acne scars becomes so relevant. By influencing both cell turnover and collagen production, retinol offers a unique dual-action approach.
The Science of Retinol: How a Vitamin A Derivative Rewires Skin Repair
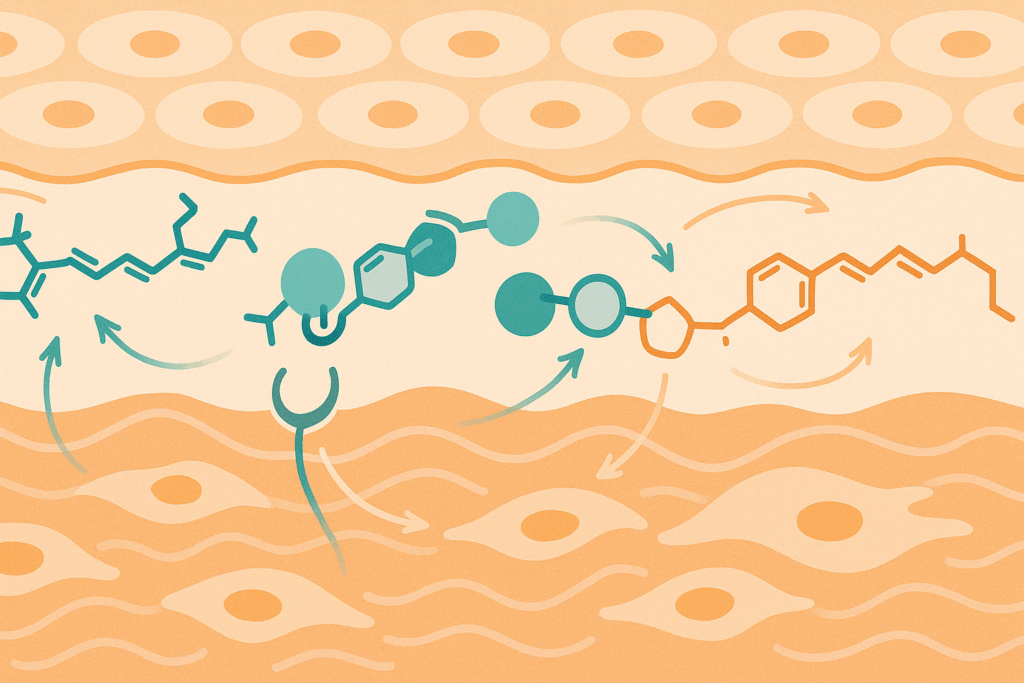
Retinol, a form of vitamin A, functions as a prodrug—it converts into retinoic acid (the active form) within the skin. This transformation sets off a cascade of biological processes that improve the skin’s regenerative capabilities. At a cellular level, retinol binds to specific nuclear receptors in skin cells, influencing gene expression. This changes how skin cells behave, encouraging faster cell turnover, reducing hyperpigmentation, and stimulating fibroblasts to produce more organized collagen.
For those wondering, “Does retinol help with acne scars?” the answer lies in this very mechanism. Faster cell turnover means that damaged, pigmented, or irregular cells are more rapidly replaced with healthier ones. In parallel, increased collagen synthesis helps to rebuild the dermal matrix that underlies atrophic scars. These two mechanisms—epidermal renewal and dermal remodeling—are what make retinol for scars such a powerful strategy.
It’s also worth noting that retinol’s anti-inflammatory properties contribute to its effectiveness. By reducing lingering subclinical inflammation around scar tissue, retinol can minimize the risk of hyperpigmentation worsening or new breakouts contributing to additional scarring. This makes it particularly beneficial when integrated into a long-term post-acne recovery regimen.

Dermatologists Weigh In: Retinol as a Gold Standard in Post-Acne Care
Ask any board-certified dermatologist about the best topical agent for acne scars, and retinol will almost certainly top the list. While other treatments like microneedling, laser resurfacing, or chemical peels may offer faster or more dramatic results, they often come with higher risks, costs, and downtime. Retinol, in contrast, provides a balance of efficacy and tolerability when used consistently over time.
Dr. Mona Gohara, associate clinical professor of dermatology at Yale School of Medicine, frequently prescribes retinol for scars in her practice. She notes that while prescription-strength tretinoin works faster, many patients achieve excellent outcomes with over-the-counter formulas—especially when used in conjunction with other supportive skincare ingredients like niacinamide and hyaluronic acid.
Another expert, Dr. Shereene Idriss, emphasizes that choosing the best retinol for acne scars isn’t just about strength. “It’s about formulation and skin compatibility,” she explains. “A well-formulated retinol pimple cream with soothing ingredients like ceramides or peptides can reduce the irritation that often discourages users from continuing treatment.”
Indeed, one of the most common pitfalls of retinol use is premature discontinuation due to peeling, redness, or dryness. Dermatologists universally stress that acclimating the skin gradually—sometimes starting with just two applications per week—is critical for long-term success.

Retinol for Scars vs. Other Treatments: What Sets It Apart
While retinol is not the only treatment for acne scars, it offers some distinct advantages. Unlike chemical exfoliants such as alpha hydroxy acids (AHAs), which work only at the surface level, retinol penetrates deeper into the dermis. This makes it particularly effective for atrophic scars, which originate in the deeper layers of the skin.
Moreover, unlike some laser or microneedling treatments, which carry a higher risk of post-inflammatory hyperpigmentation—particularly in skin of color—retinol has a more favorable risk profile. It can be safely used on all Fitzpatrick skin types, though it must still be introduced carefully and always paired with broad-spectrum sun protection.
Another differentiator is accessibility. Many formulations of retinol for acne scars are available without a prescription, making them a more affordable and practical long-term option. Brands like Differin (adapalene) have gained FDA approval for over-the-counter use and provide retinoid-based therapy at a fraction of the cost of in-office procedures.
Ultimately, what makes retinol unique is its ability to provide both preventive and reparative benefits. When used consistently, it not only softens the appearance of existing scars but also helps prevent new ones by reducing breakouts and mitigating inflammation. This dual role is why many dermatologists recommend it as a foundational component of acne aftercare.

Choosing the Best Retinol for Acne Scars: What to Look For
With an overwhelming number of products on the market, choosing the best retinol for acne scars can feel daunting. However, several criteria can help guide your decision. First and foremost is the strength and type of retinoid. Over-the-counter options typically contain retinol, retinyl palmitate, or retinaldehyde, while prescription formulas may contain tretinoin, tazarotene, or adapalene.
Formulation matters as much as strength. A poorly formulated product—even with a high retinol percentage—may cause more irritation than improvement. Look for retinol pimple creams that include stabilizing and soothing agents, such as glycerin, niacinamide, or panthenol, which help the skin tolerate retinoids more effectively. Products packaged in opaque, air-tight containers are also more likely to maintain the stability of the retinol, which degrades quickly when exposed to light and air.
Another consideration is time-release technology. Encapsulated retinol, which is delivered gradually over time, tends to cause less irritation and may be a better option for those with sensitive or compromised skin barriers. These formulations help users stick with the treatment long enough to see meaningful results—typically within 12 to 24 weeks.
Many dermatologists recommend combining retinol with supportive treatments, such as azelaic acid or vitamin C, though not necessarily used at the same time. Each ingredient targets a different aspect of scarring—retinol for collagen synthesis, azelaic acid for hyperpigmentation, and vitamin C for antioxidant protection—creating a synergistic effect when used properly in rotation.

Integrating Retinol Into a Scar-Healing Routine: Best Practices for Success
To maximize results and minimize irritation, dermatologists recommend a phased approach when introducing retinol for scars. The first step involves skin preparation. Strengthening the skin barrier with ceramide-based moisturizers or niacinamide serums before initiating retinol use can reduce the risk of adverse reactions. Starting with a lower concentration—typically 0.25% to 0.5% retinol—is advisable, especially for those with sensitive skin or a history of eczema.
Application technique also matters. Retinol should always be applied at night, as UV exposure can degrade its potency and increase the risk of irritation. Users should cleanse the skin, allow it to dry fully (as damp skin can intensify retinol absorption), then apply a pea-sized amount to the entire face. Following with a gentle, non-comedogenic moisturizer can buffer potential dryness without compromising efficacy.
Sun protection is non-negotiable. Retinol makes the skin more photosensitive, and unprotected exposure can negate any progress made, potentially worsening hyperpigmentation. A broad-spectrum sunscreen with SPF 30 or higher is essential every morning—even on cloudy days or when staying indoors, as UVA rays can penetrate windows.
Patience is key. While some individuals may notice smoother skin or a more even tone within a few weeks, significant improvement in acne scars generally takes at least three to six months of consistent use. Documenting progress with monthly photographs can help users stay motivated, as daily changes may be too subtle to notice.
Does Retinol Help with Acne Scars Long-Term? What the Research Says
The question “Does retinol help with acne scars long-term?” has been the subject of multiple clinical studies, many of which confirm its efficacy. A 2016 review published in the Journal of Cosmetic Dermatology analyzed several randomized controlled trials and found that retinoids significantly improved atrophic acne scars, particularly when used for more than 12 weeks. The authors noted that collagen remodeling was evident on histological examination, affirming that the effects were not just superficial.
Another study conducted in 2020 found that participants using a 0.5% retinol cream for 24 weeks experienced a statistically significant reduction in scar depth and skin roughness, with minimal side effects. Improvements were more pronounced in patients who used retinol in conjunction with other barrier-supportive ingredients, such as ceramides and hyaluronic acid.
These findings reinforce what dermatologists have long observed in clinical practice: that retinol for acne scars delivers cumulative, long-lasting benefits. However, they also underscore the importance of consistent use and appropriate product formulation. Retinol is not a quick fix, but rather a gradual, sustainable solution that aligns with the skin’s natural regeneration cycle.
Psychological Benefits of Treating Acne Scars: More Than Skin Deep
The impact of acne scars extends beyond the skin’s surface. Numerous studies have linked visible scarring with diminished self-esteem, social anxiety, and even symptoms of depression. For many individuals, the emotional weight of acne scars can be heavier than that of the original acne itself. In this context, using retinol for scars is not just a cosmetic decision—it’s a mental health intervention.
When people begin to see tangible improvements in their skin texture or tone, they often report feeling more confident, less anxious, and more willing to engage socially. This psychological shift can ripple outward, improving professional performance, relationships, and overall well-being. While it’s important not to equate physical appearance with self-worth, helping individuals feel comfortable in their skin is a meaningful component of holistic health care.
Mental health professionals often emphasize the role of agency in psychological recovery. When patients take control of their skin care—using evidence-based products like retinol pimple creams—they are engaging in a proactive form of self-care that reinforces a sense of empowerment. In this way, skin health and mental health become closely intertwined, particularly for those recovering from acne.
Frequently Asked Questions: Retinol for Acne Scars
1. How do I know if retinol is actually improving my acne scars or just irritating my skin?
It can be difficult to distinguish between retinol’s initial irritation and true progress when treating acne scars. In the early weeks, redness and mild peeling are expected and may resemble a flare-up, but these symptoms usually subside within four to six weeks. Improvements in skin texture—such as smoother-feeling skin or shallower atrophic scars—often become noticeable after eight to twelve weeks of consistent use. A useful way to track whether retinol for acne scars is working is by taking monthly photos under the same lighting, focusing on subtle shifts in tone and scar depth. If inflammation or dryness worsens over time instead of improving, it could indicate a need to adjust your formula or frequency, rather than discontinuing altogether. In these cases, switching to a gentler retinol pimple cream or using barrier-repair moisturizers in tandem may help you continue reaping the benefits without excessive irritation.
2. Can retinol worsen acne scars before making them better?
Yes, in some cases, retinol may seem to worsen the appearance of acne scars before improvements become visible—a phenomenon sometimes called the “retinol purge.” This occurs because retinol for acne scars accelerates cell turnover, which can bring dormant microcomedones to the surface, temporarily increasing breakouts. This purge is not a sign that retinol doesn’t work; in fact, it often precedes clearer, smoother skin. While this stage may feel discouraging, most dermatologists recommend continuing with a consistent routine unless the reaction becomes severe. To reduce the likelihood of worsening scars during this adjustment period, many experts advise starting with a low-strength retinol pimple cream and applying it only twice weekly before building up tolerance.
3. Is there a difference between prescription retinoids and over-the-counter retinol when it comes to treating scars?
There is a clinically significant difference between over-the-counter (OTC) and prescription-grade retinoids, especially in terms of speed and intensity of results. Prescription options like tretinoin or tazarotene are more potent and convert directly into retinoic acid, making them faster-acting agents for addressing deep acne scars. However, OTC products that contain stabilized retinol or retinaldehyde may be more appropriate for sensitive skin types due to their slower conversion rates and lower irritation potential. For many users, the best retinol for acne scars is one they can use consistently without side effects, regardless of whether it’s OTC or prescription. In some cases, layering OTC retinol for scars with ingredients like peptides, azelaic acid, or alpha hydroxy acids can approximate the results of stronger formulas over time.
4. What role does skin type play in the effectiveness of retinol for acne scars?
Skin type plays a crucial role in both how retinol works and how well it is tolerated. People with oily or combination skin may be able to tolerate higher concentrations of retinol for acne scars, while those with dry or sensitive skin may require slower-release formulations or buffered products. Fitzpatrick skin type also matters: individuals with medium to deep skin tones may be more prone to post-inflammatory hyperpigmentation (PIH), meaning that formulations targeting both discoloration and texture—such as a retinol pimple cream combined with niacinamide—may offer broader benefits. Those with rosacea-prone or eczema-prone skin should approach retinol for scars cautiously, beginning with the lowest strengths and gradually titrating upward. Understanding your skin’s baseline resilience and barrier function is essential when determining the best retinol for acne scars in a personalized treatment plan.
5. Can retinol help with the red or brown marks left behind after acne clears?
Absolutely. One of the lesser-known benefits of retinol for acne scars is its impact on residual pigment changes—specifically, post-inflammatory erythema (PIE) and post-inflammatory hyperpigmentation (PIH). While not technically “scars,” these marks can linger for months and be just as distressing. Retinol accelerates epidermal turnover, helping discolored skin cells shed more quickly while simultaneously downregulating melanocyte activity responsible for producing excess pigment. In this context, the best retinol for acne scars may be one that includes additional antioxidants or tyrosinase inhibitors to prevent rebound pigmentation. For those especially concerned with dark marks, combining retinol with azelaic acid or tranexamic acid (in alternating routines) may speed up pigment clearance without compromising skin health.
6. Are there any cutting-edge advancements in retinol delivery for scar treatment?
Yes, innovations in retinol delivery systems have expanded the landscape of scar treatment considerably. Modern formulations often utilize encapsulated or microencapsulated retinol, which allows the active ingredient to be released slowly over time, minimizing irritation while preserving potency. Some of the best retinol for acne scars now incorporate liposomal delivery, ensuring deeper dermal penetration with less surface-level inflammation. Additionally, newer dual-phase systems combine retinol with soothing compounds that are activated upon application, creating a buffer effect that supports long-term adherence. These advances allow even those with previously intolerant skin to benefit from the collagen-stimulating effects of retinol for scars. As this area evolves, we may see formulations tailored to specific scar types—such as rolling versus boxcar scars—emerge in the clinical dermatology market.
7. Can I use retinol for acne scars if I’m still experiencing active breakouts?
Yes, and in many cases, it’s actually advisable. Retinol for acne scars also addresses acne itself by preventing clogged pores, reducing oil production, and calming inflammation. However, when active acne and scarring coexist, it’s important to tailor your routine to prevent exacerbation. A non-comedogenic, gel-based retinol pimple cream can help address both concerns simultaneously without overwhelming the skin. For inflammatory acne, consider combining retinol with a benzoyl peroxide wash in the morning and retinol at night—though not in the same routine, as the ingredients can deactivate each other. When breakouts subside, the retinol already integrated into your regimen will continue helping with scar repair, making the transition from acne treatment to scar management more seamless.
8. How can I combine retinol with in-office treatments for faster scar reduction?
Retinol can be used synergistically with many in-office treatments to accelerate scar improvement. Procedures like microneedling, fractional laser therapy, and chemical peels often create controlled skin injury to stimulate collagen production. When retinol is used leading up to or after these treatments—with appropriate downtime—it enhances results by priming the skin and extending the rejuvenation process. That said, dermatologists typically recommend pausing retinol use for several days before and after aggressive procedures to minimize irritation. The best retinol for acne scars in this context is often a post-procedural formulation, sometimes prescribed in conjunction with stem cell serums or growth factors to support recovery. This layered approach can significantly reduce both atrophic scars and residual pigment within a shorter timeframe.
9. What are the psychological benefits of improving acne scars with retinol over time?
Addressing acne scars with retinol may offer significant psychological benefits that extend far beyond skin appearance. Clinical psychology research increasingly supports the connection between skin condition and self-esteem, especially among those recovering from persistent or disfiguring acne. As skin clarity improves through the consistent use of retinol for scars, individuals often report increased confidence, reduced social anxiety, and greater comfort in personal and professional settings. This gradual yet visible transformation can help shift one’s internal narrative from one of shame or embarrassment to empowerment and self-care. Many patients describe using the best retinol for acne scars as part of a broader journey toward reclaiming their sense of identity, especially when they’ve previously felt defined by their skin issues.
10. How long should I realistically use retinol before expecting permanent scar improvement?
Retinol is a long-term commitment when it comes to treating acne scars. While some improvements in skin tone and smoothness may appear within 6 to 12 weeks, significant changes in scar structure—such as shallower atrophic scars—typically take 6 to 12 months of consistent use. This timeline is comparable to that of in-office treatments but carries fewer risks and costs. Because retinol for acne scars promotes collagen production over time, the improvements tend to be gradual but long-lasting. The best retinol for acne scars is one that fits seamlessly into your lifestyle and routine, allowing for uninterrupted use. For ongoing benefits, many dermatologists recommend continuing retinol even after visible scar resolution, both as a preventive measure and as part of an overall skin maintenance plan.
The Bottom Line: Why Retinol Remains a Cornerstone in Acne Scar Treatment
Despite the ever-expanding list of cosmetic procedures and trendy ingredients, retinol continues to stand the test of time. For those asking, “Does retinol help with scars, and is it worth the commitment?” the answer, according to both dermatologists and science, is a resounding yes. Its ability to stimulate collagen, normalize pigmentation, reduce inflammation, and improve overall skin texture makes it one of the most versatile tools in dermatology.
Choosing the best retinol for acne scars means considering more than just strength—it involves understanding formulation, delivery method, skin compatibility, and long-term skin goals. Retinol isn’t a miracle overnight cure, but its gradual, accumulative effects make it a worthwhile investment for anyone seeking to restore not just the look but also the feel and function of their skin after acne.
For those still uncertain, consulting a dermatologist can provide clarity and personalization, ensuring that your choice of retinol for acne scars aligns with your unique skin needs. Whether used alone or as part of a broader skin-healing routine, retinol remains a scientifically backed, dermatologist-approved ally in the ongoing pursuit of healthier, scar-free skin.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Retinol: Cream, Serum, What It Is, Benefits, How To Use
Acne Scars: Treatment, Removal, Best, and More
Retinol For Scarring And Post Acne Marks
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.